Follow Us
© 2025 All Rights Reserved
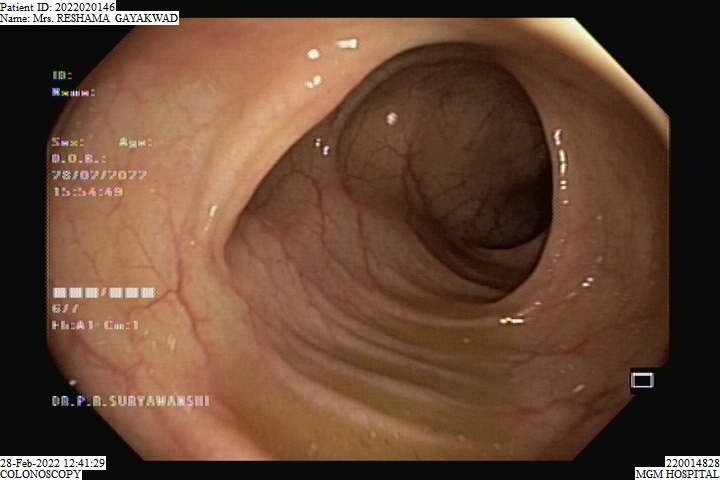
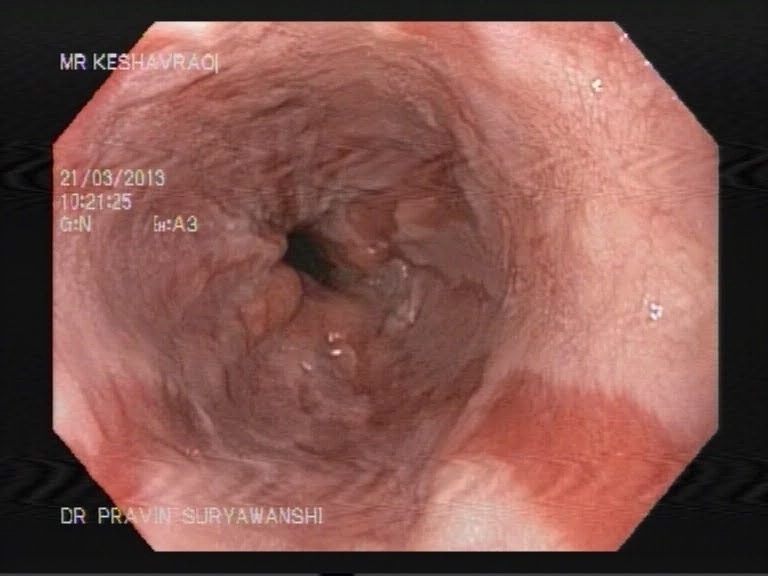
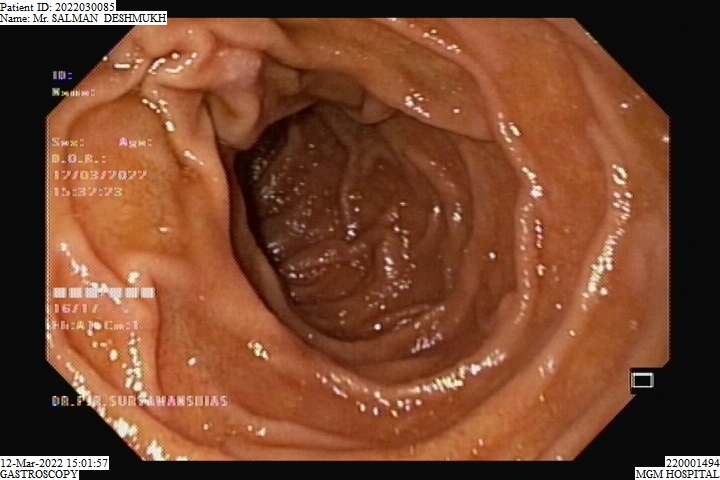
A colonoscopy is a procedure done to examine the colon and a part of the small intestine by a long, thin and flexible tube with a camera at the end of it. It helps your doctor detect any polyps, bleeding sites like ulcers and cancer of the colon. A colonoscopy is usually a day care procedure where the patient arrives in the morning undergoes the colonoscopy and can be sent home the same day.
Preparation for a colonoscopy includes drinking a laxative preparation and remaining empty stomach for at least 6 hours before the procedure. The patients are usually asked to mix the laxative in 2 liters of water and drink it over two hours. This will cause watery stool and have a purgatory effect leading to cleaning of the colon. This step makes it easier for your doctor to examine the colon properly as it ensures all the fecal matter has been cleared out.
The patient is usually sedated during a colonoscopy and usually does not feel any pain or discomfort during the procedure. The patient may experience some bloating or nausea after the procedure, which is normal and usually subsides in a few hours. The procedure itself takes about 15-20 mins but the patient can take upto 1-2 hours to recover from the sedation.

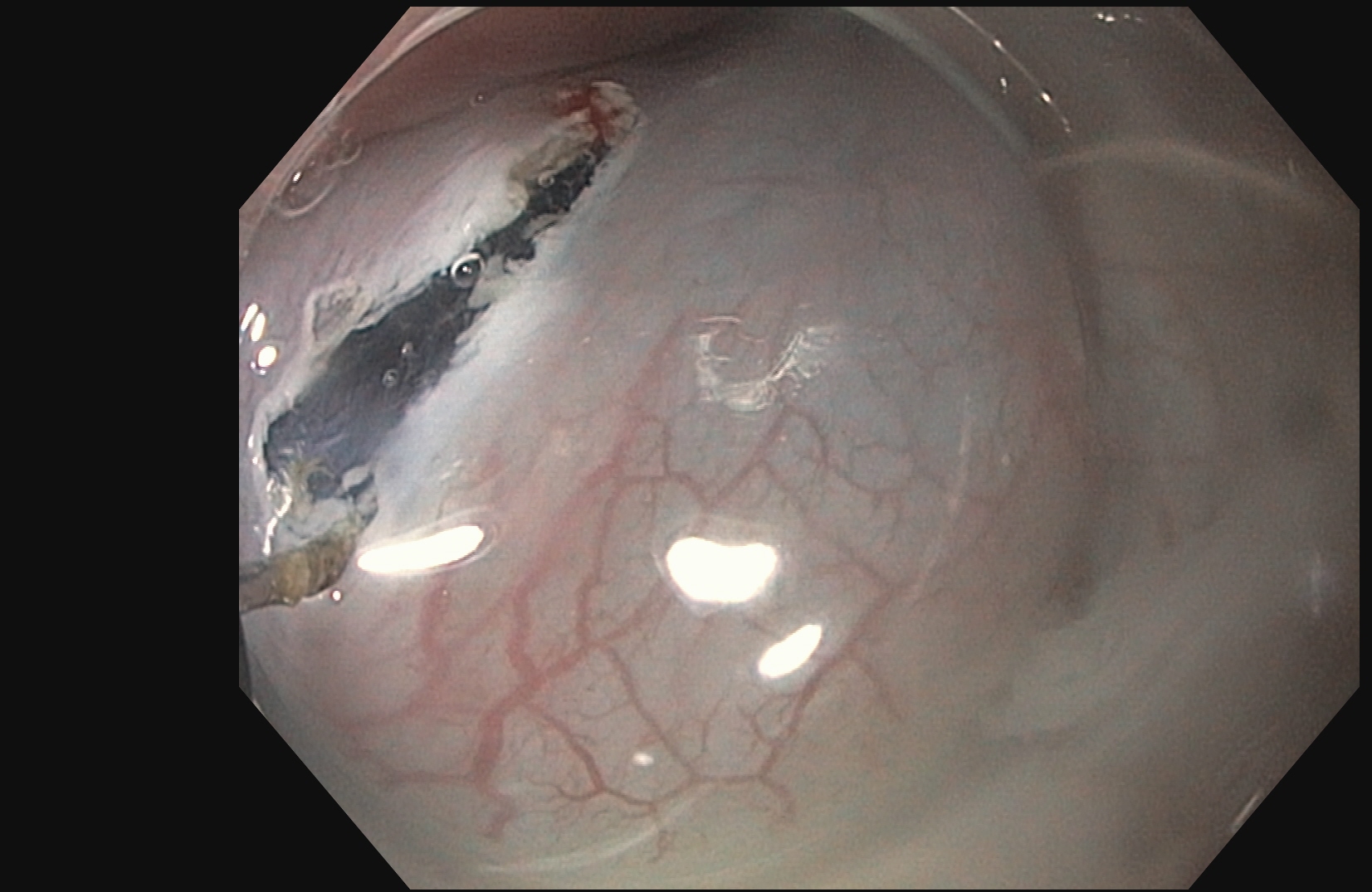
ESD is an advanced endoscopic procedure used to remove gastrointestinal tumors that have not entered the muscle layer. ESD may be done in the esophagus, stomach or colon.Under anesthesia, a long narrow tube is passed through the throat to reach the lesion in the stomach, or the tube is passed through the anus to reach the lesion in the colon.
The procedure consists of three steps:
You will be asked to change into a gown before the procedure. You will be given a sedative and you will not experience any sensation of gagging or choking. A mouthpiece will be placed between your teeth to protect your mouth. The endoscope will be passed through your mouth and into the esophagus, stomach and duodenum. The procedure usually takes 30-45 mins and the patient is usually sent home on the same day.
EMR is a minimally invasive, endoscopic removal of benign and early malignant lesions in the gastrointestinal (GI) tract.
This procedure is performed with a long, narrow tube equipped with a light, video camera and other instruments. During endoscopic mucosal resection of the upper digestive tract, the tube is passed down your throat to reach an abnormality in your esophagus, stomach or upper part of the small intestine (duodenum). When EMR is used to remove lesions from the colon, the tube is guided up through the anus.
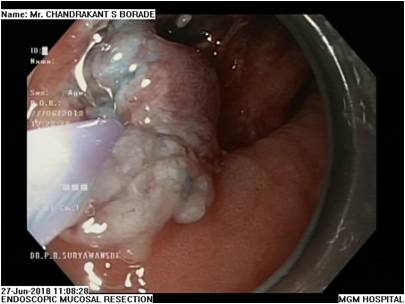



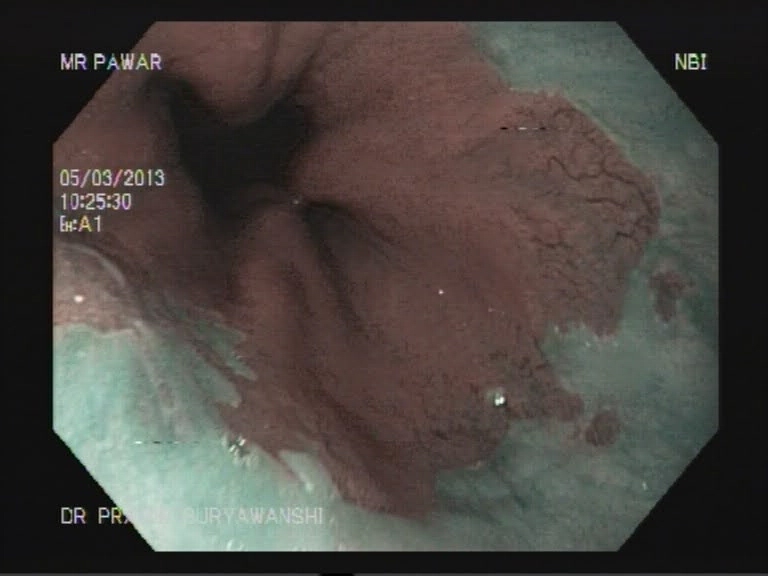
EMR is used for patients with discrete nodules in an area of Barrett’s mucosa. This is a safe and effective way to remove precancerous and early cancerous lesions. When EMR is performed in the esophagus, you will need to go home on certain medications to help your esophagus heal.
Stomach
EMR is used in the stomach in order to remove early gastric cancers.
Duodenum
EMR is used in the duodenum to resect duodenal polyps.
Colon
EMR is used to resect rectal and colon polyps.
The patient prepares for the procedure by remaining empty stomach for atleast 6 hours before the procedure. EMR usually takes about 30 mins to 1 hour and the patient is usually sent home on the same day.
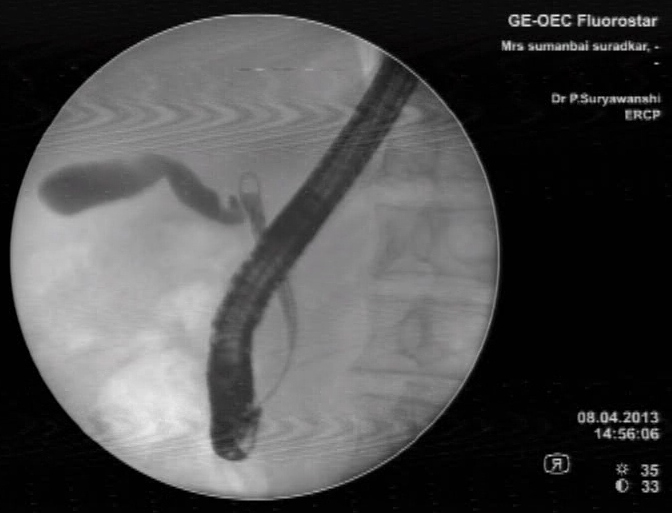
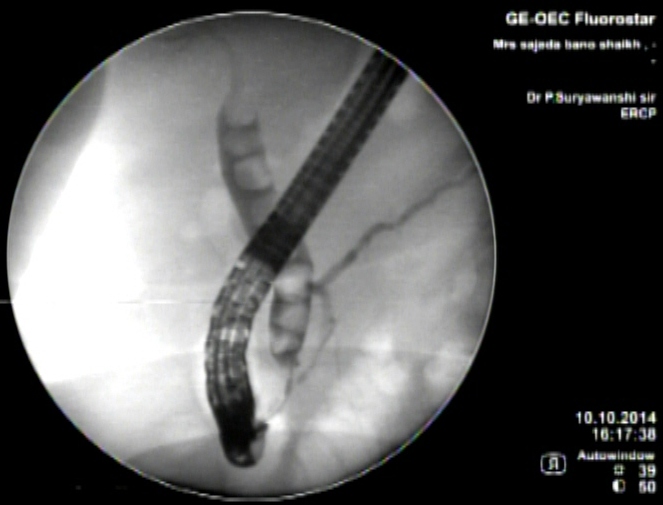
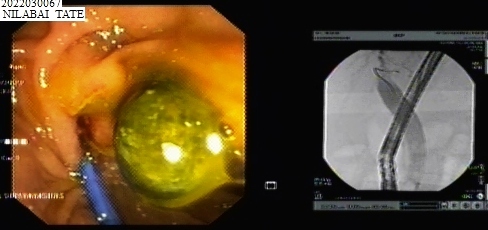
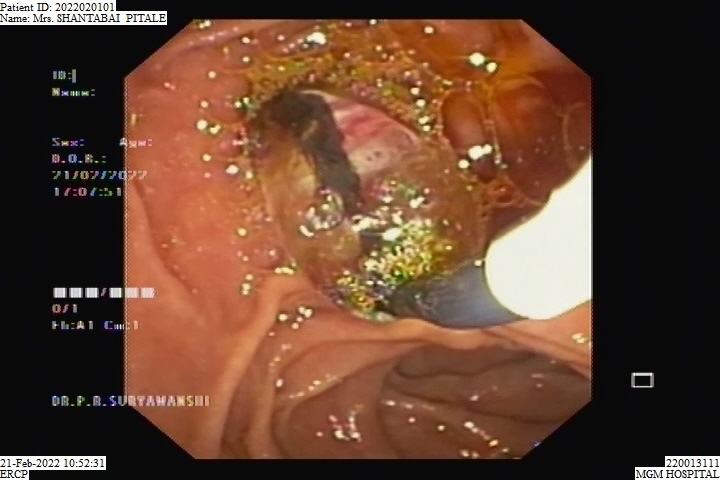
ERCP stands for endoscopic retrograde cholangiopancreatography. As hard as this is to say, the idea behind the exam is fairly simple. A dye is injected into the bile and pancreatic ducts using a flexible, video endoscope. Then x-rays are taken to outline the bile ducts and pancreas.
An ERCP uses x-ray and is performed in a room specially equipped for x-rays. The patient is positioned on his or her stomach or left side with the head turned to the right. The patient is sedated and a piece of plastic placed in the mouth to keep the mouth open. The endoscope is then gently inserted into the upper esophagus. The patient breathes easily throughout the exam, with gagging rarely occurring. A thin tube is inserted through the endoscope to the main bile duct entering the duodenum. Dye is then injected into this bile duct and/or the pancreatic duct and x-ray films are taken. If a gallstone is found, steps may be taken to remove it. An incision can be made using electrocautery (electrical heat) to open the lower portion of the duct as it enters the duodenum. Additionally, it is possible to widen narrowed ducts and to place small tubing, called stents, in these areas to keep them open. The exam takes from 20 to 40 minutes, but could take up to an hour or more, depending on the complexity of the procedure, after which the patient is taken to the recovery area.The patient prepares for the procedure by remaining empty stomach for at least 6 hours before the procedure and the patient is usually sent home the same day.


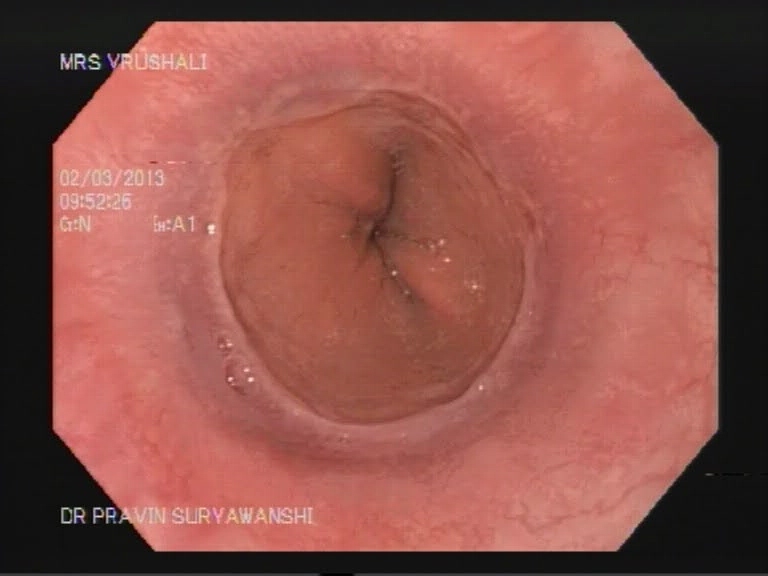
A upper GI scopy is a procedure done to examine the esophagus, stomach and a part of the small intestine by a long, thin and flexible tube with a camera at the end of it. It helps your doctor detect any polyps, bleeding sites like ulcers and cancer of the GI tract. An upper GI scopy is usually a day care procedure where the patient arrives in the morning, undergoes the scopy and can be sent home the same day. The throat is anesthetized by a spray or sometimes the patient is even sedated to relax the patient.
The procedure takes from 15 to 30 minutes, after which the patient is taken to the recovery area. There is no pain with the procedure and patients seldom remember much about it. The patient prepares for the procedure by remaining empty stomach for atleast 6 hours before the procedure and the patient is usually sent home the same day.
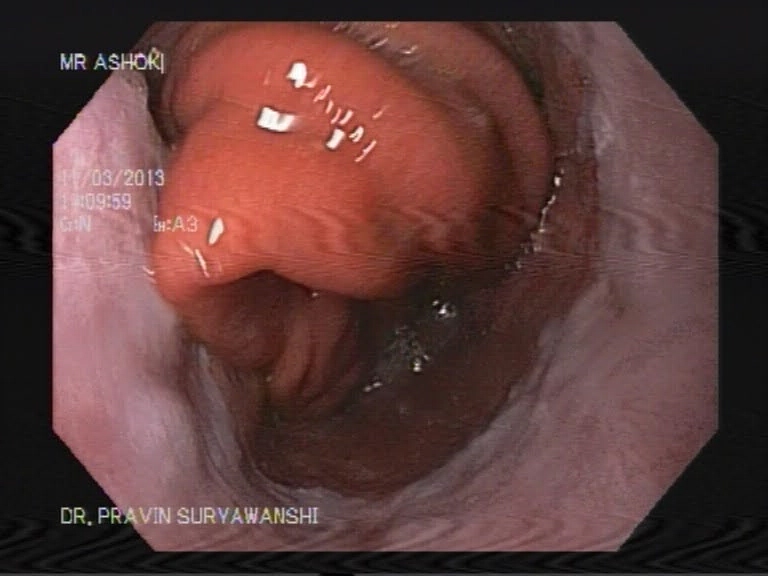
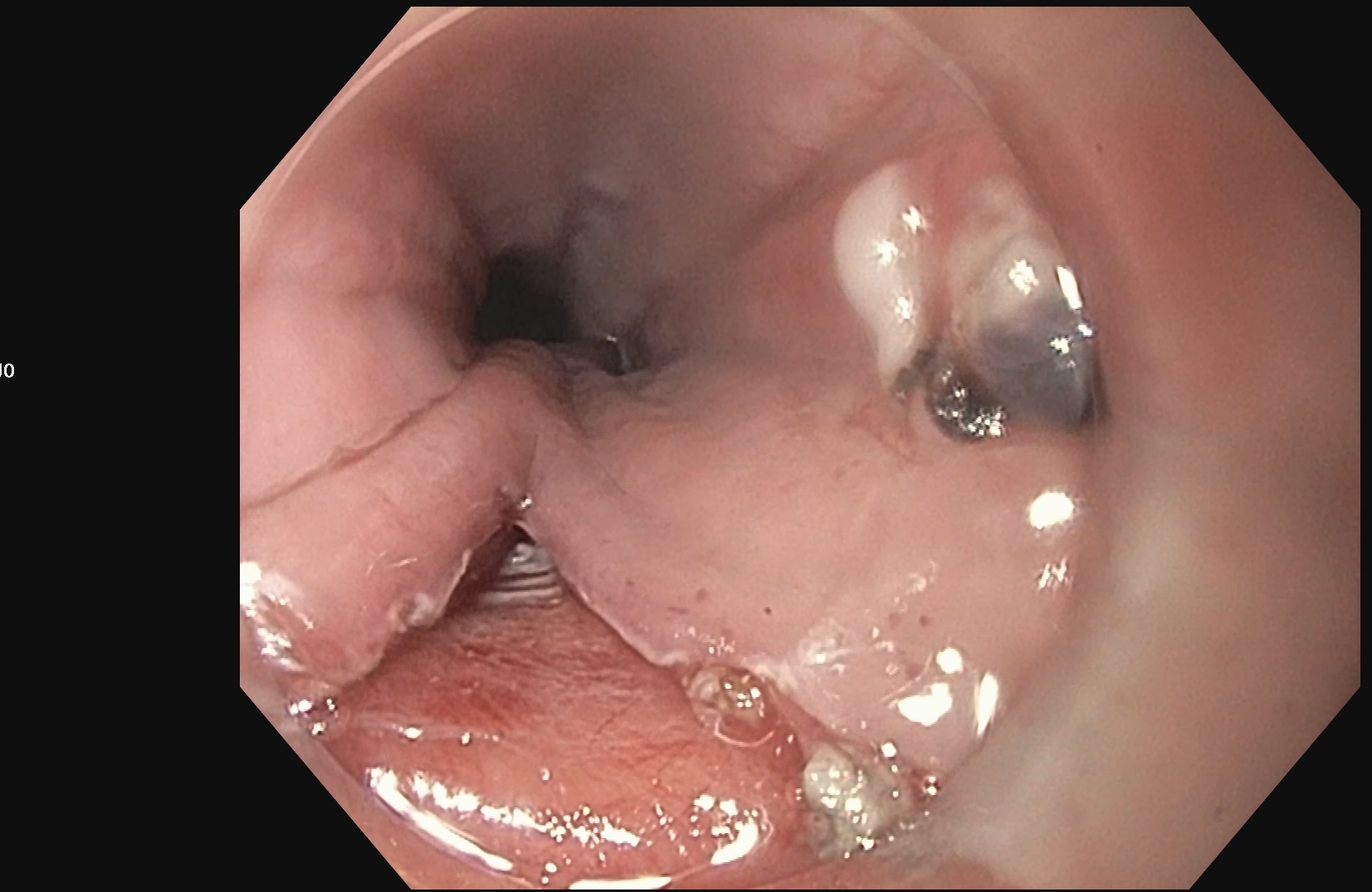
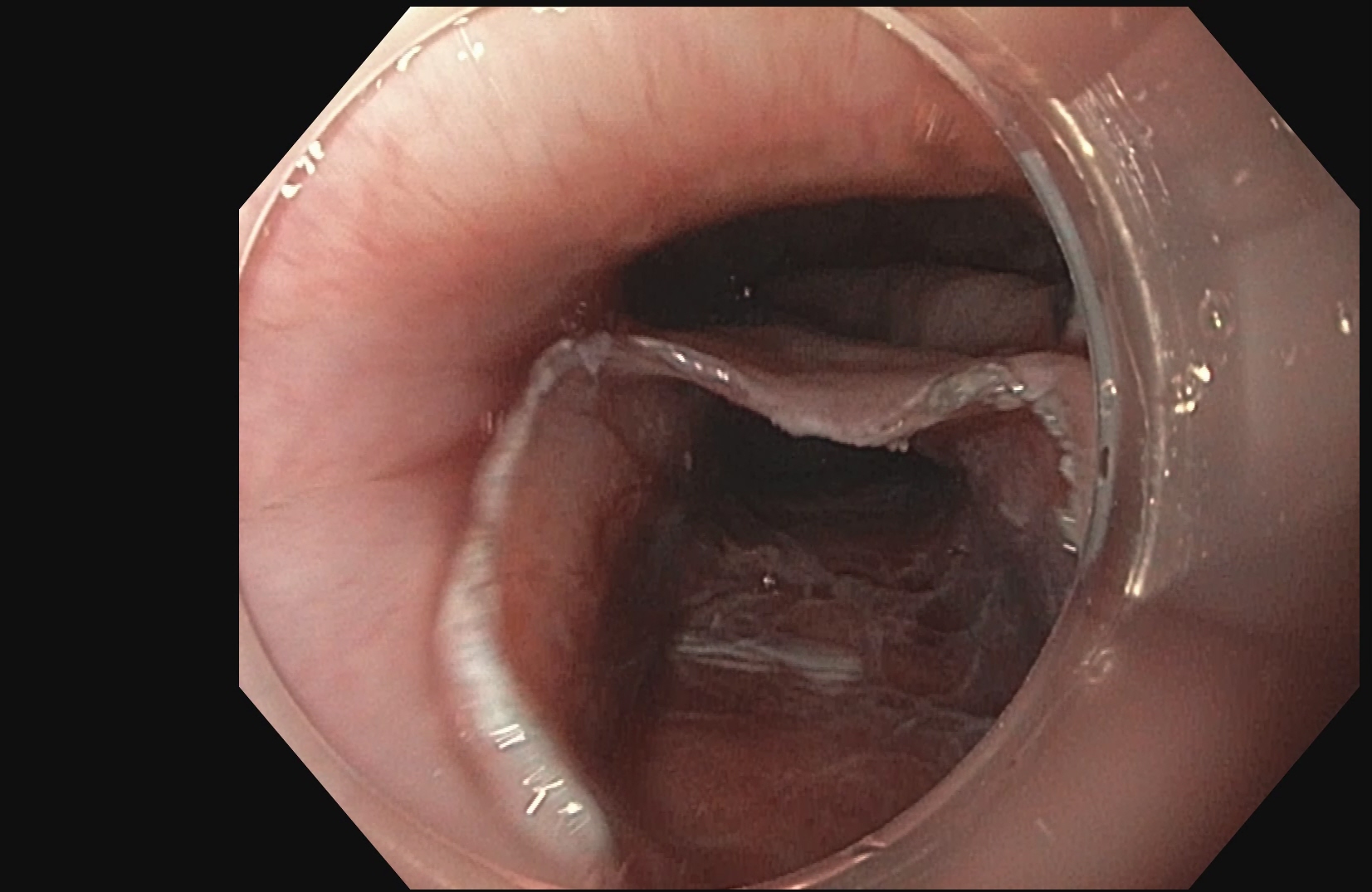
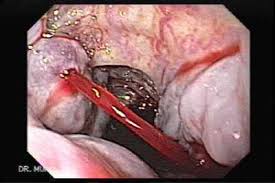
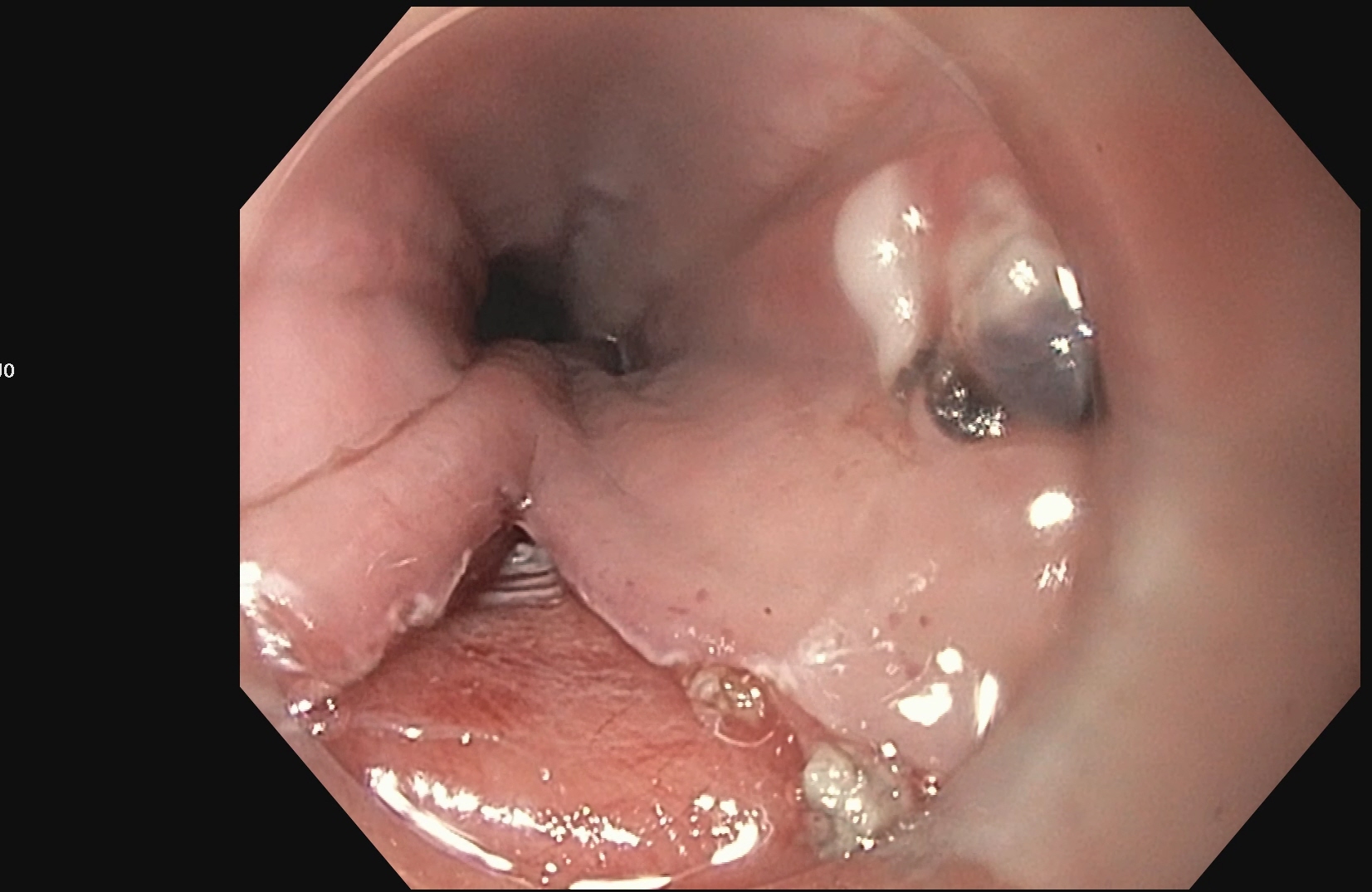
Esophageal Variceal Banding is used to treat enlarged veins in the esophagus, the tube connecting the throat to the stomach. If left untreated esophageal veins (varices) can spontaneously rupture and cause severe bleeding.The procedure is performed during an upper gastrointestinal endoscopy. A local anesthetic is given to numb the throat and sedation medication will also be given through IV to help you relax/sleep through the procedure.
A scope is placed in the mouth down to the esophagus. When varices are found, tiny elastic bands are placed around the enlarged veins in the esophagus to tie them off, so they can’t bleed. The banded varices are then eventually sloughed after a few days and the esophagus is much less likely to bleed after it’s healed.


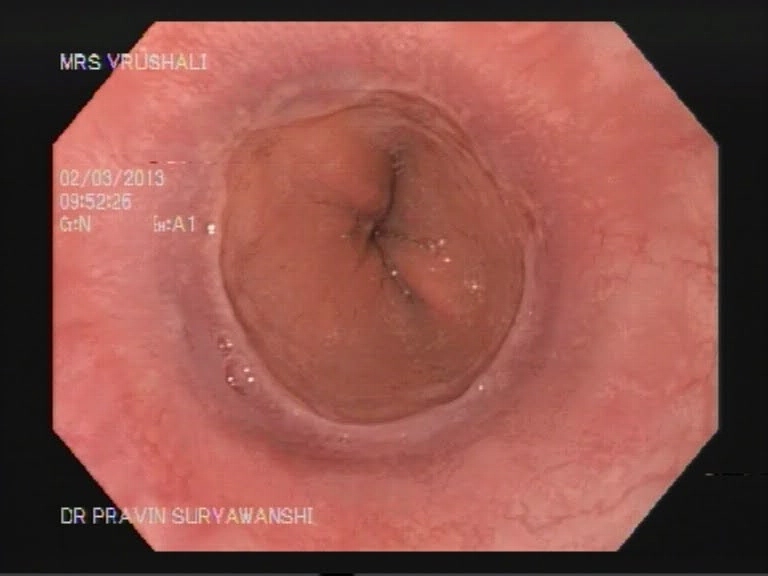
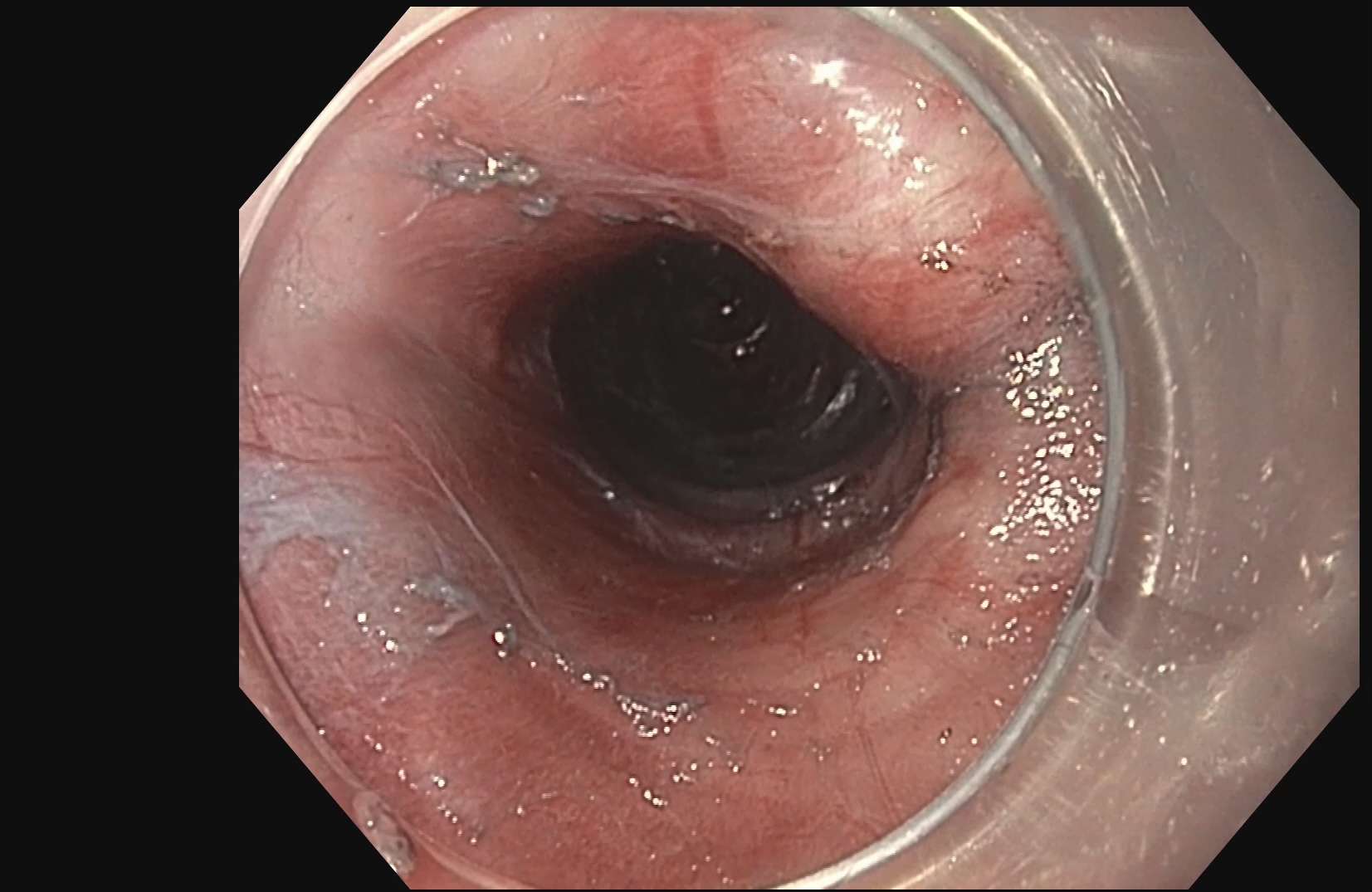
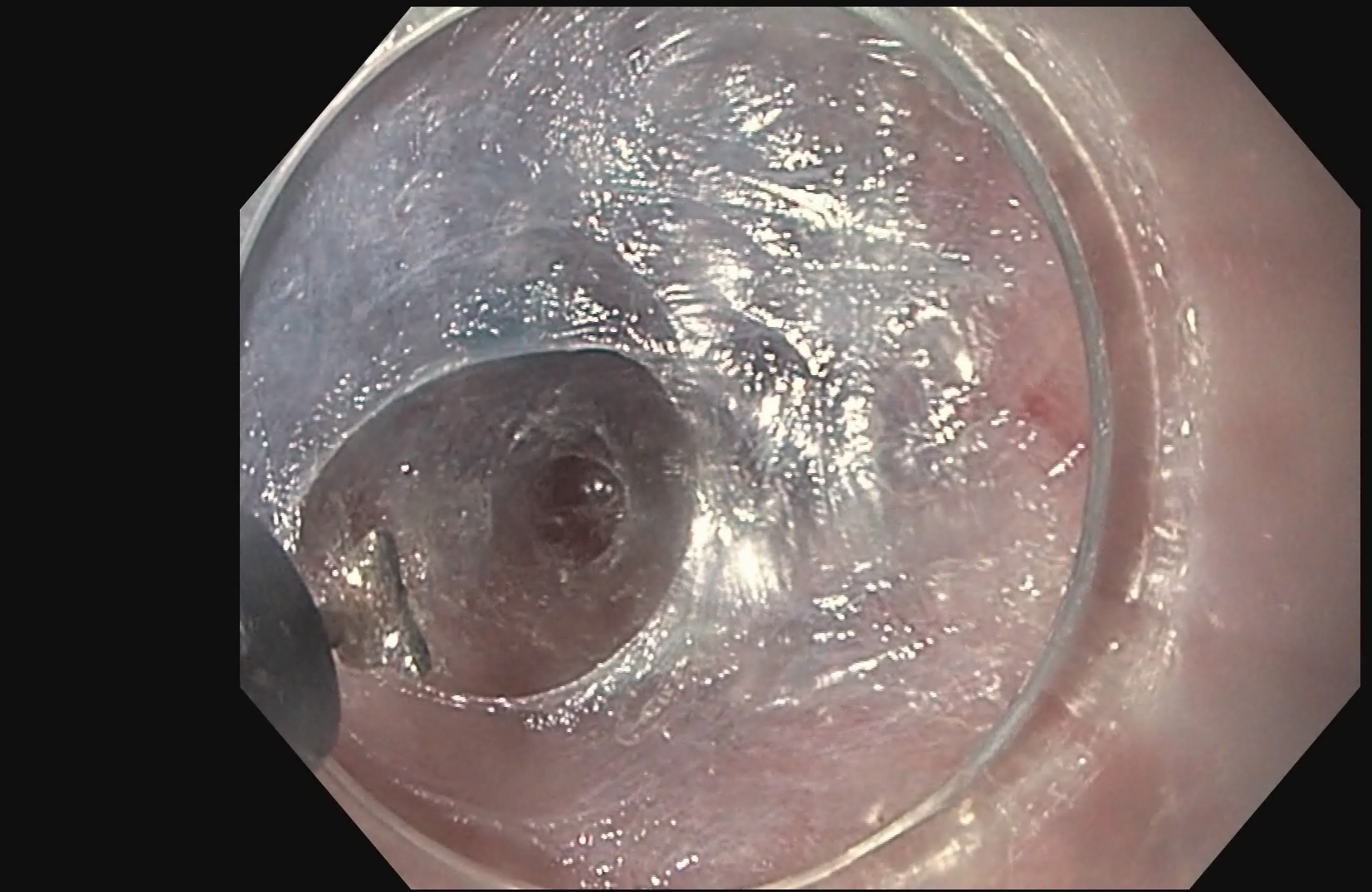
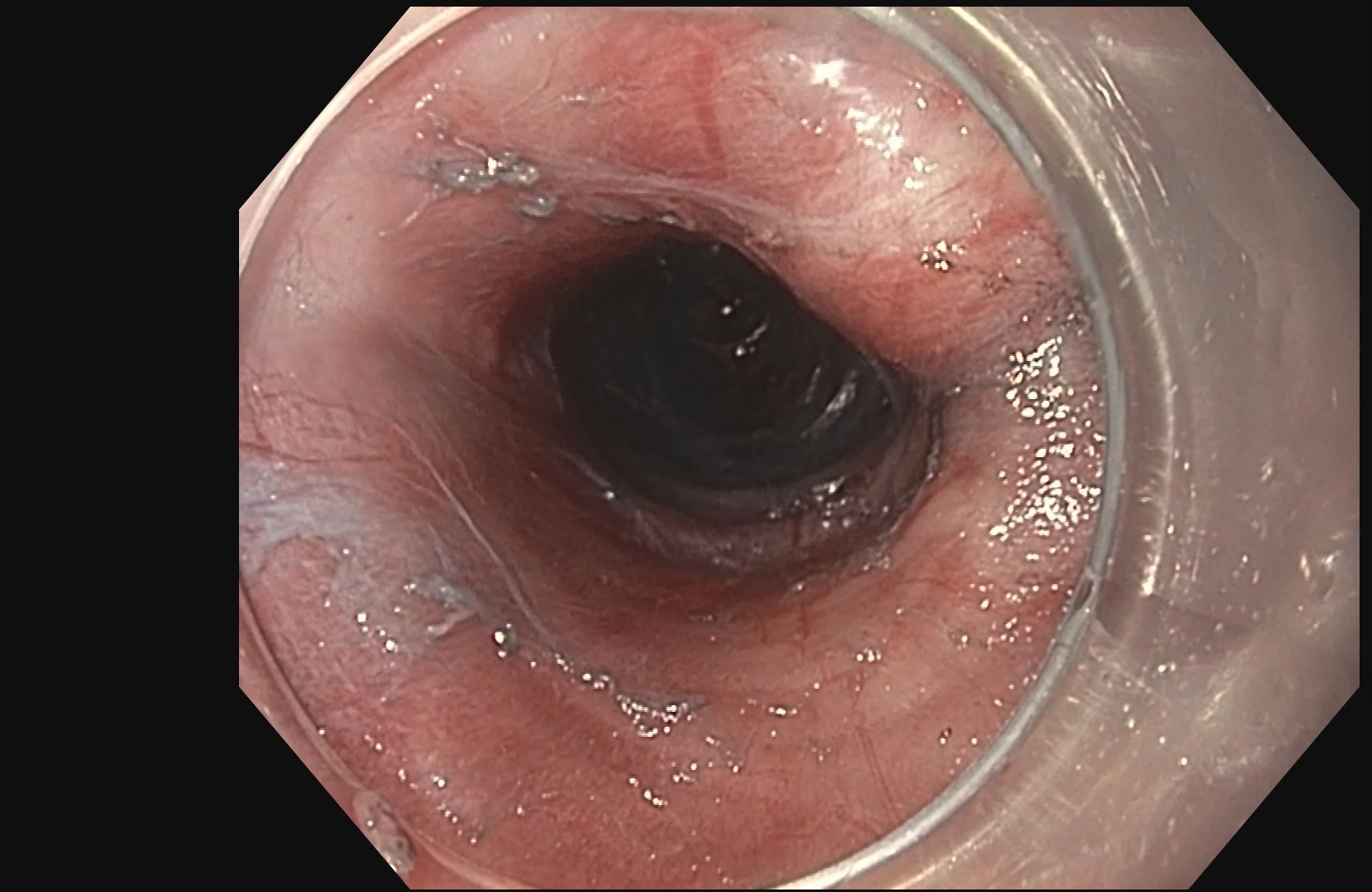
The esophagus is the long, narrow food tube (gullet) that carries food and liquid from the mouth to the stomach. It can become blocked or injured in a variety of ways. Esophageal dilatation is the technique used to stretch or open the blocked portion of the esophagus. The method most commonly used for esophageal dilatation is balloon dilators.Balloon dilators – Deflated balloons are placed through the endoscope and across the stricture. When inflated, they become sausage shaped, stretch, and break the stricture.
Simple balloon dilatation, which is the most common technique used, may take only 20 to 30 minutes. Recovery is usually quick and the patient can soon begin eating and drinking to test the effectiveness of the treatment. The patient prepares for the procedure by remaining empty stomach for at least 6 hours before the procedure and the patient is usually sent home the same day.
The procedure takes about one hour from start to finish. While seated in a chair or lying on the side, thin soft tubing is gently passed through the nose, or occasionally the mouth. Upon swallowing, the tip of the tube enters the esophagus and the technician then quickly passes it down to the desired level. During the exam, the technician usually asks the patient to swallow saliva (called a dry swallow) or water (called a wet swallow). Pressure recordings are made and the tubing is withdrawn. Patients can usually resume regular activity, eating, and medicines immediately after the exam.

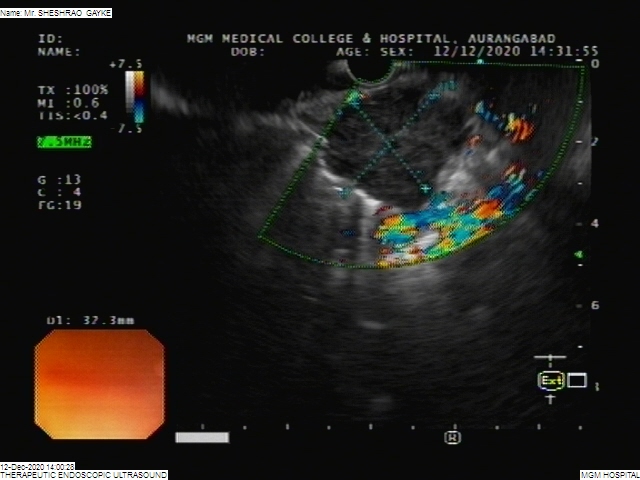

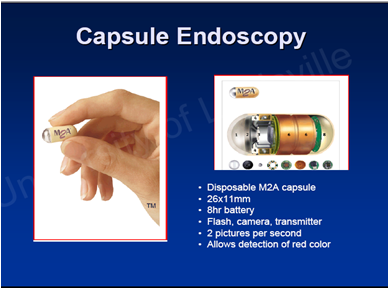
Endoscopic ultrasound (EUS) is a minimally invasive procedure to assess digestive (gastrointestinal) and lung diseases. A special endoscope uses high-frequency sound waves to produce detailed images of the lining and walls of your digestive tract and chest, nearby organs such as the pancreas and liver, and lymph nodes.
When combined with a procedure called fine-needle aspiration, EUS allows your doctor to sample (biopsy) fluid and tissue from your abdomen or chest for analysis. EUS with fine-needle aspiration can be a minimally invasive alternative to exploratory surgery.EUS techniques are also used in certain treatments, such as draining pseudocysts.
During EUS your doctor passes a thin, flexible tube (endoscope) through your mouth and through your digestive tract. A small ultrasound device (transducer) in the tube produces sound waves that create a precise image of surrounding tissue, including lymph nodes in the chest. The endoscope is then gradually withdrawn.If you have fine-needle aspiration with EUS, your doctor may need to pass a second, curved device through a channel in the endoscope into your digestive tract. That device can guide a very slender needle to your lymph nodes and tumors or other abnormalities. The needle extracts fluid and tissue for analysis.EUS with fine-needle aspiration generally lasts less than an hour and the patient can be sent home the same day.
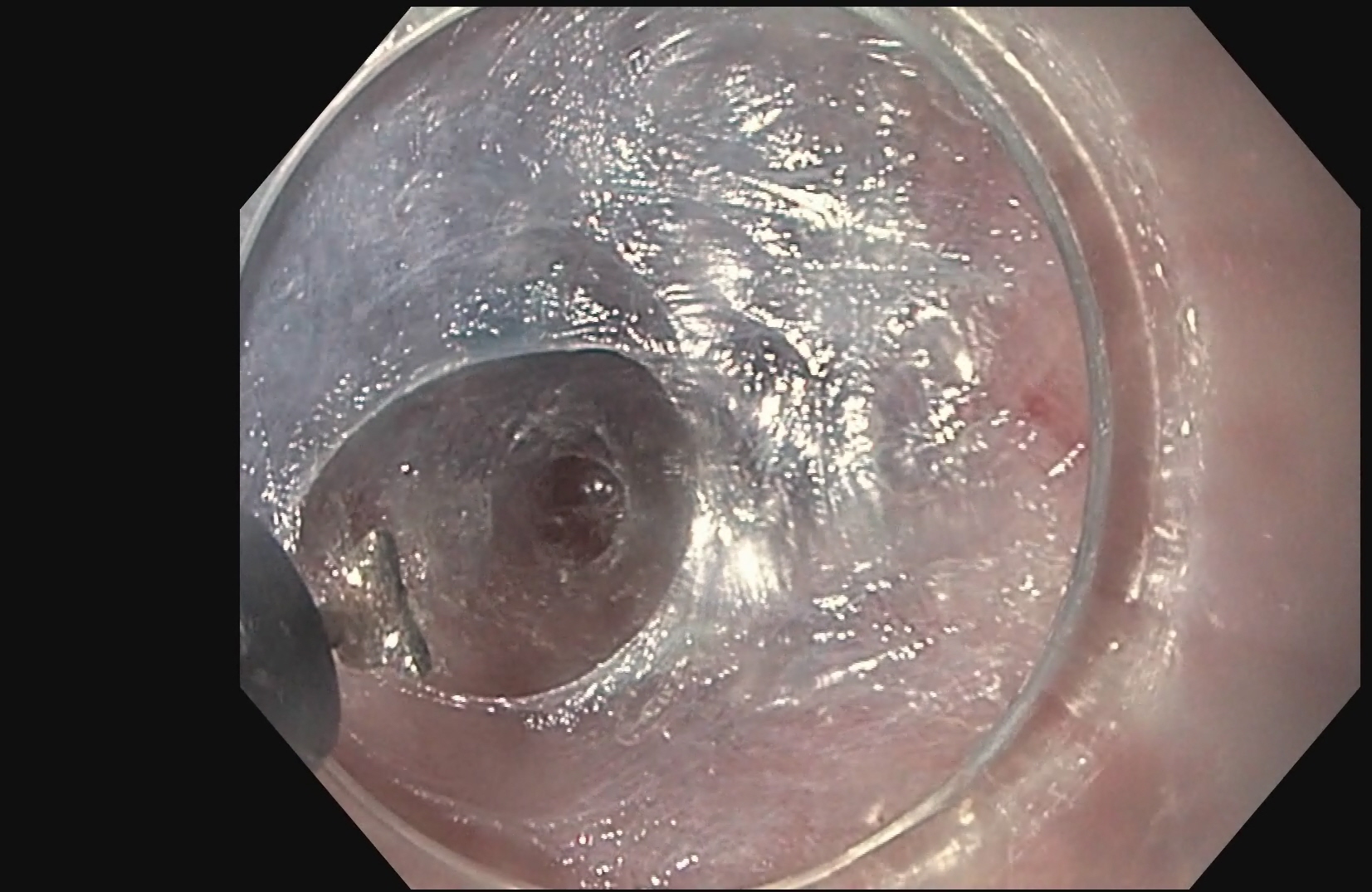
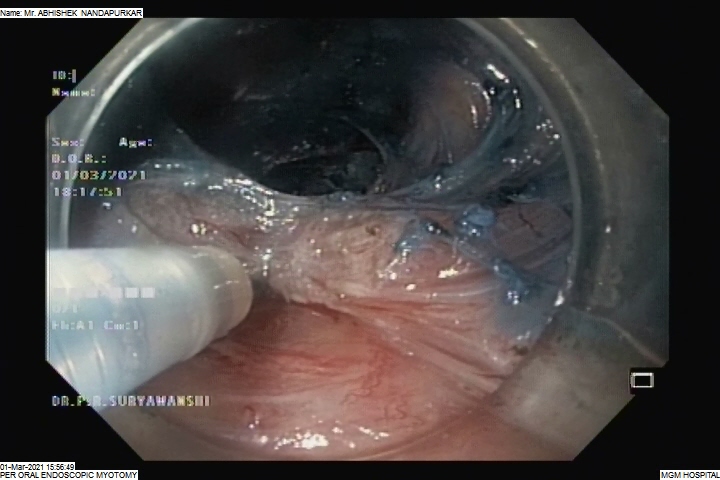
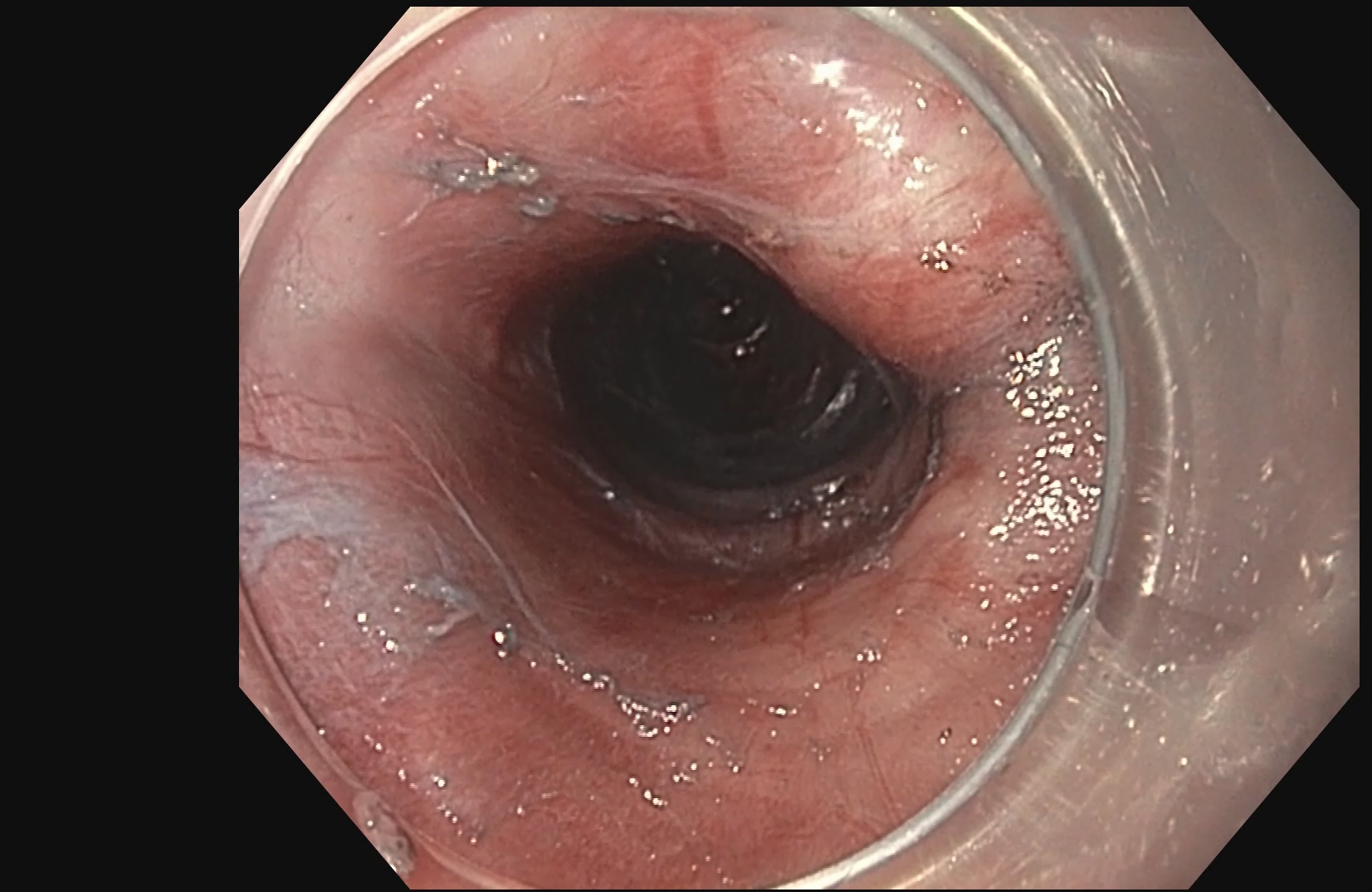
POEM is a form of third space endoscopy and endoscopic surgery. Like the traditional surgical myotomy, the procedure is performed under general anesthesia. The remainder of the procedure is performed using a flexible endoscope inserted through the mouth, and no cuts are made on the chest or abdomen. First, a submucosal injection of dyed saline creates a cushion, then a cut is made in the esophageal mucosa using electrocautery roughly 13-15 centimeters before the lower esophageal sphincter. Then, using hydrostatic dissection and electrocautery, the submucosal tunnel is made. Once the circular fibers of the lower esophageal sphincter are encountered, they are divided using electrocautery all the way down onto the first part of the stomach. This functionally weakens the sphincter, allowing improved passage of food and liquid into the stomach. Finally, the submucosal flap is closed using clips placed through the endoscope.
The procedure takes roughly 1 ½ hours but can vary on physician and patient characteristics. Patients usually spend 2–5 days in the hospital before going home. Patients may return to work and full activity immediately upon discharge from the hospital.
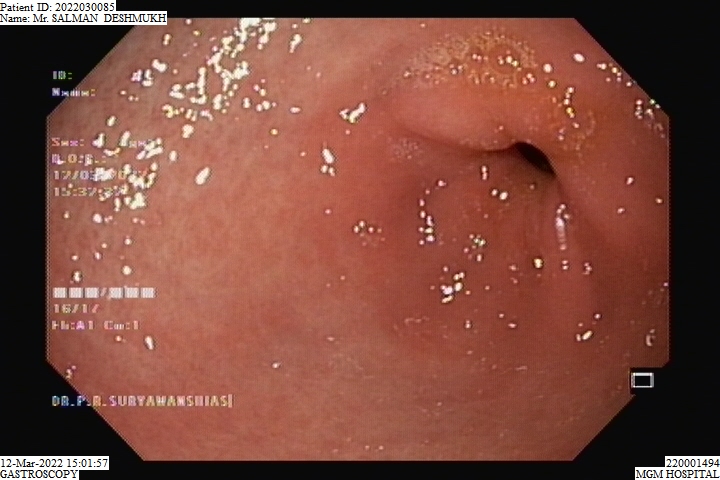

Gastroscopy
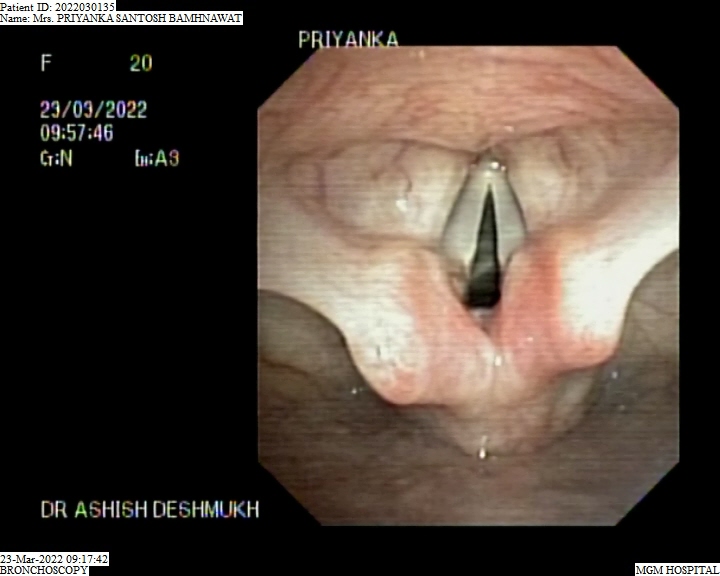

Bronchoscopy
COLONIC POLYPECTOMY

Esophageal Dilatation

Endoscopic Balloon Dilatation

Esophageal Variceal Banding
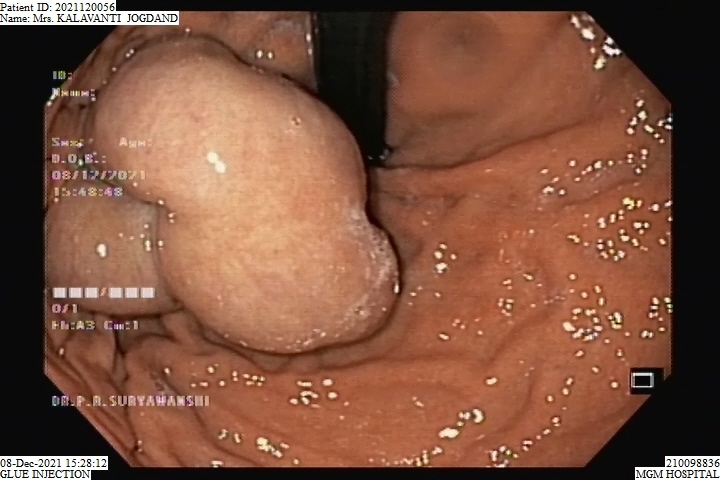
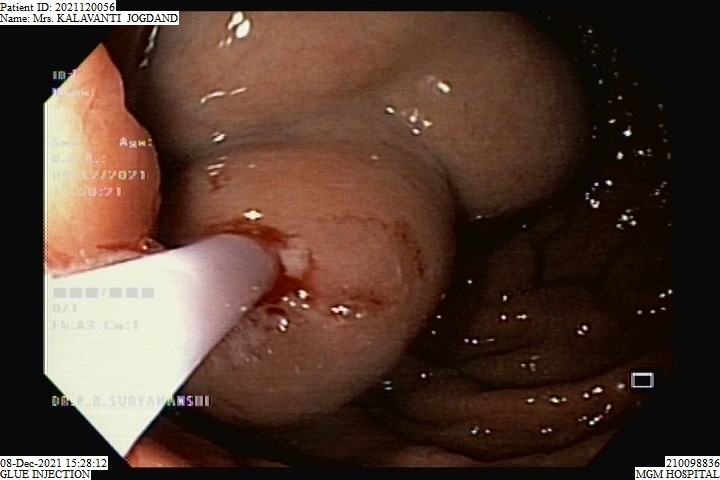
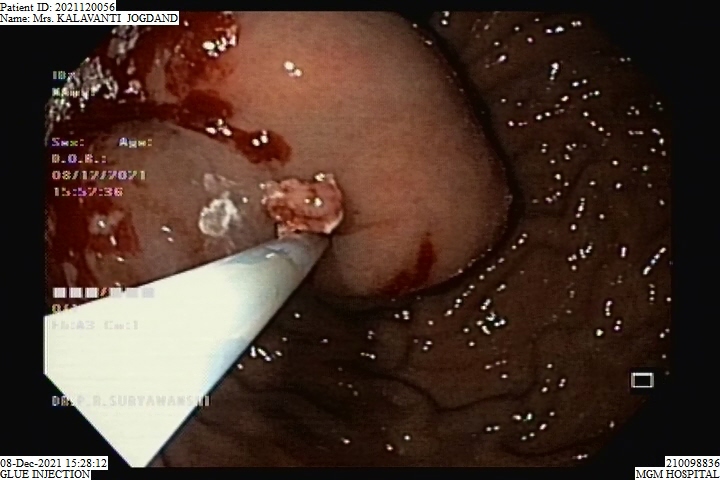
Glue Injection Procedure

Esophageal Manometry
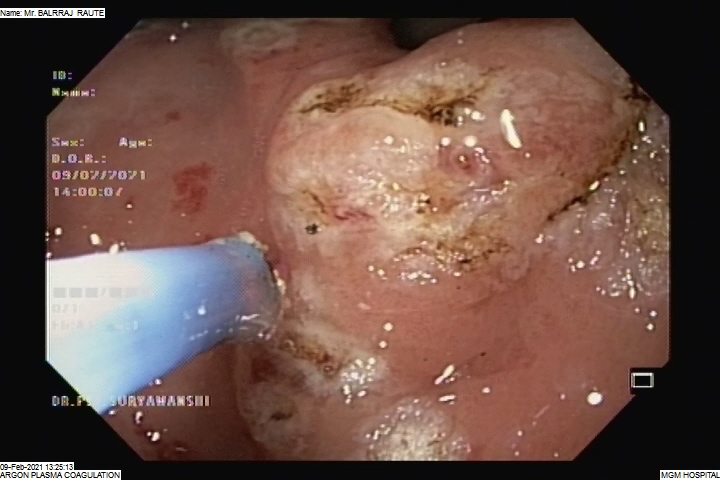
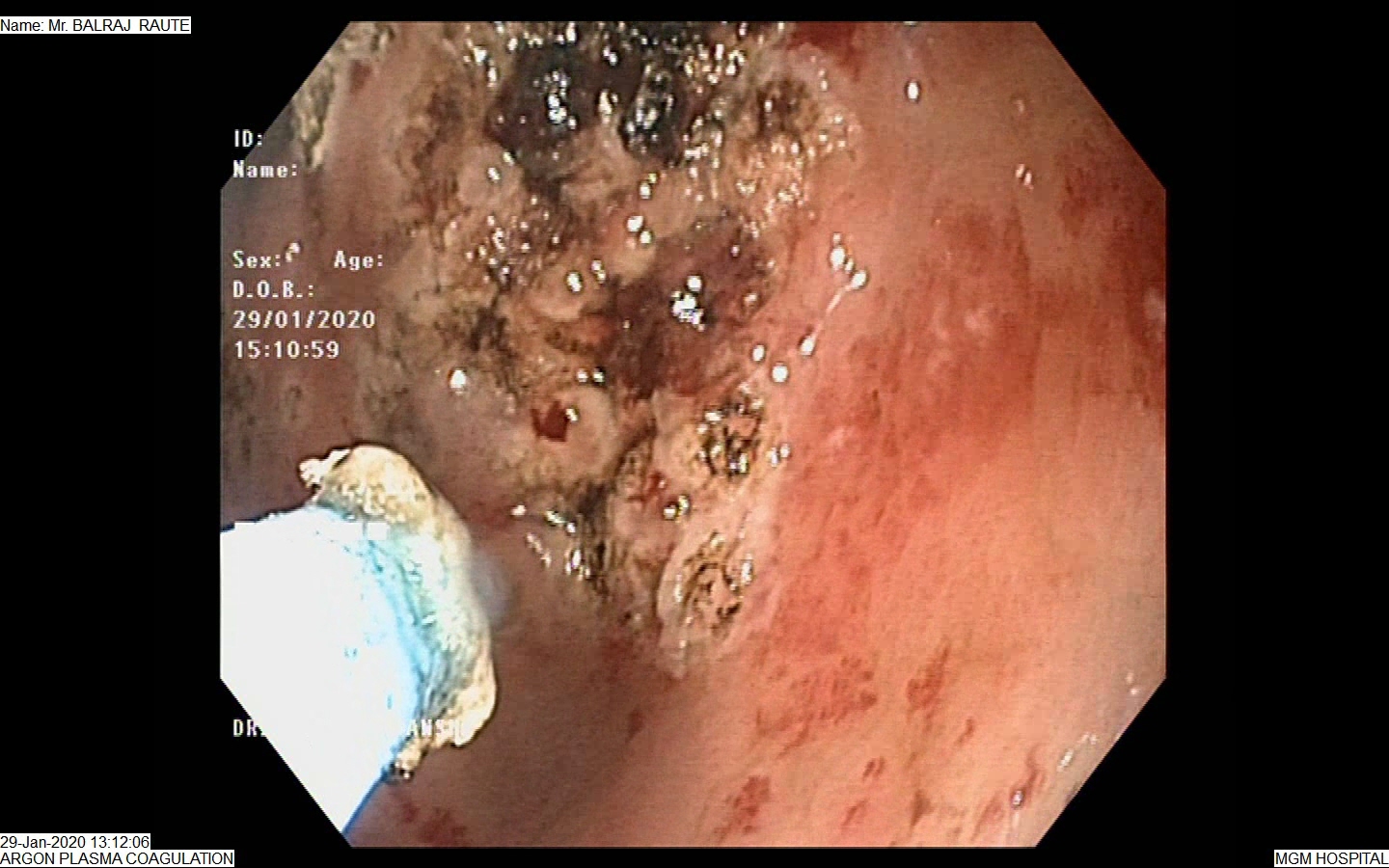
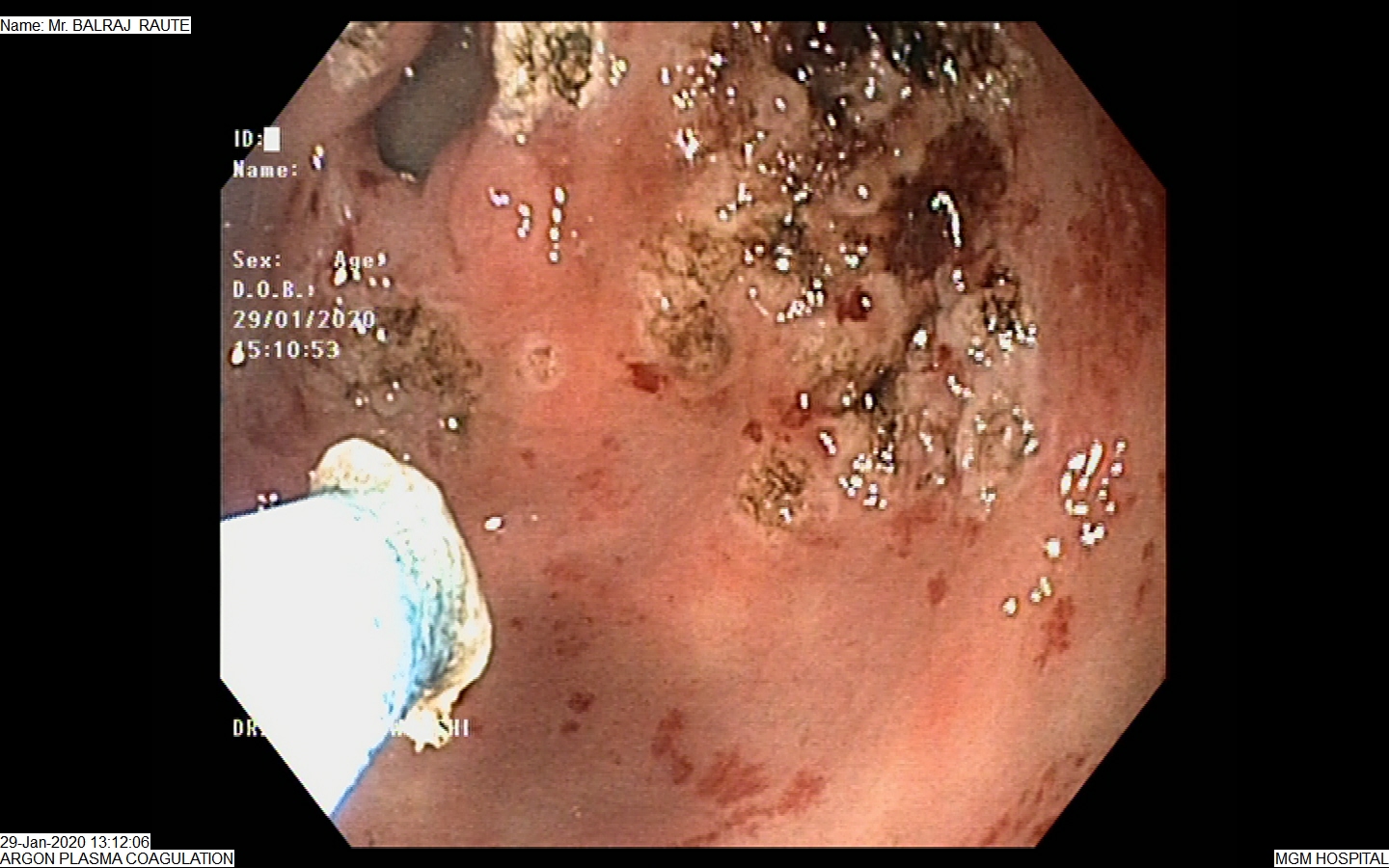
APC – (Argon Plasma Coagulation)


BALLOON SPHINCTEROPLASTY
POEM (Per Oral Endoscopic Myotomy)
Sigmoidoscopy
Endoscopic Polypectomy
Gastroscopy with Polypectomy
Endoscopic RT Insertion
C-Arm Guided Procedure
Malecot’s Catheter
Endoscopic PEG Removal
Endoscopic Ultrasound (EUS) Guided Celiac Block
Side Viewing Endoscopy (Duodenoscopy)
Haemoclip Application
Mechanical Lithotripsy for CBD Stone
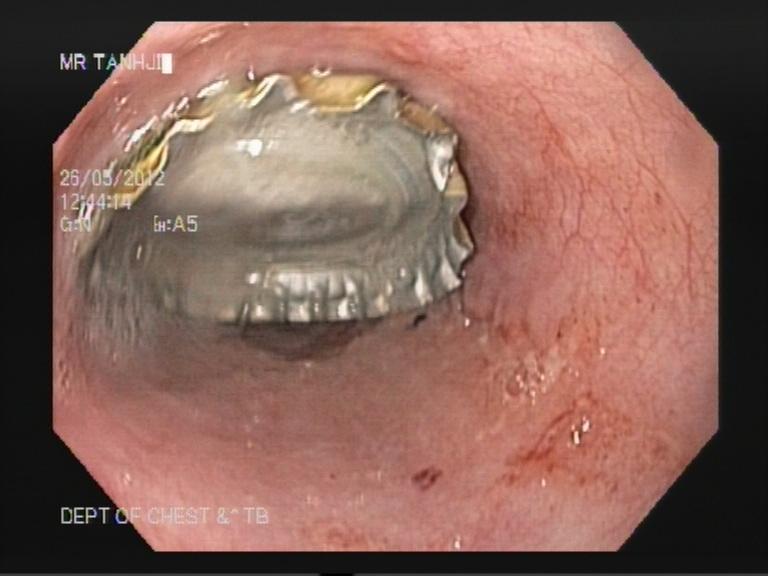
Oesophageal Metallic Stenting
Endoscopic Mucosal Resection (EMR)
Rectal Manometry
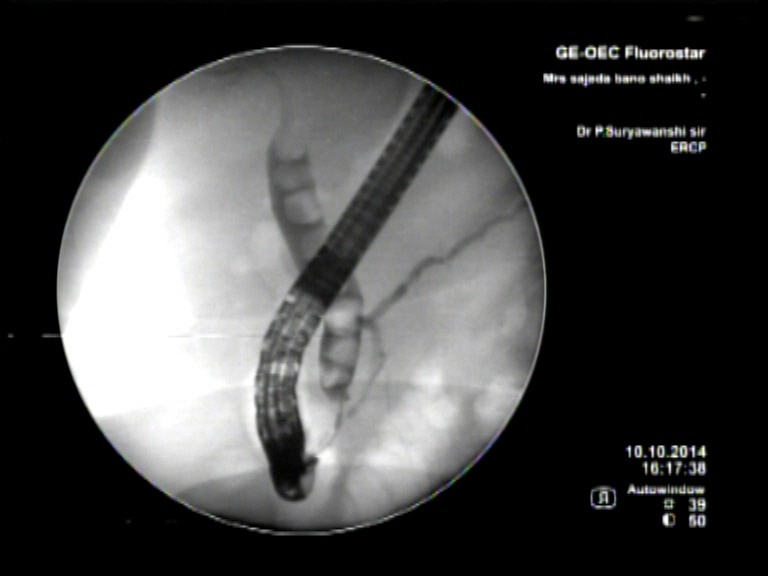



Endoscopic Retrograde Cholangiopancreaticography is a minimally invasive procedure that is helpful in diagnosing and treating disorders of the gallbladder, liver and the pancreas. A contrast dye and X-Ray studies are used to highlight the network of ducts that are part of the hepatobiliary network. The sphincter formed at the site where the ducts open into the duodenum is located and dye is injected to study the biliary tract or to look for any obstruction. Sometimes the sphincter is cut to release obstruction or to remove stone. Obstruction of the flow of bile due to stricture formation or other reasons responds well to sphincterotomy.
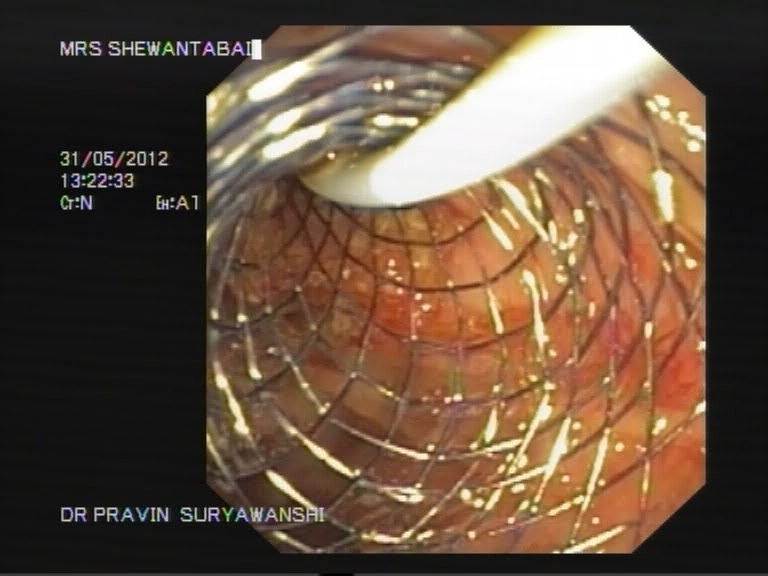
Bile duct stenting is a surgical procedure during which a collapsible stent is used to maintain a patent bile duct. The surgeon will use minimally invasive techniques to locate the site of obstruction of the bile duct. A stent is inserted inside the bile duct under endoscopic guidance. The stent releases the obstruction of the bile duct and prevents the collapsing of the duct walls. Symptoms of jaundice following biliary obstruction respond well to bile duct stenting. It is also commonly used for small stones in CBD prior to Laparoscopic Cholecystectomy for gallstones.
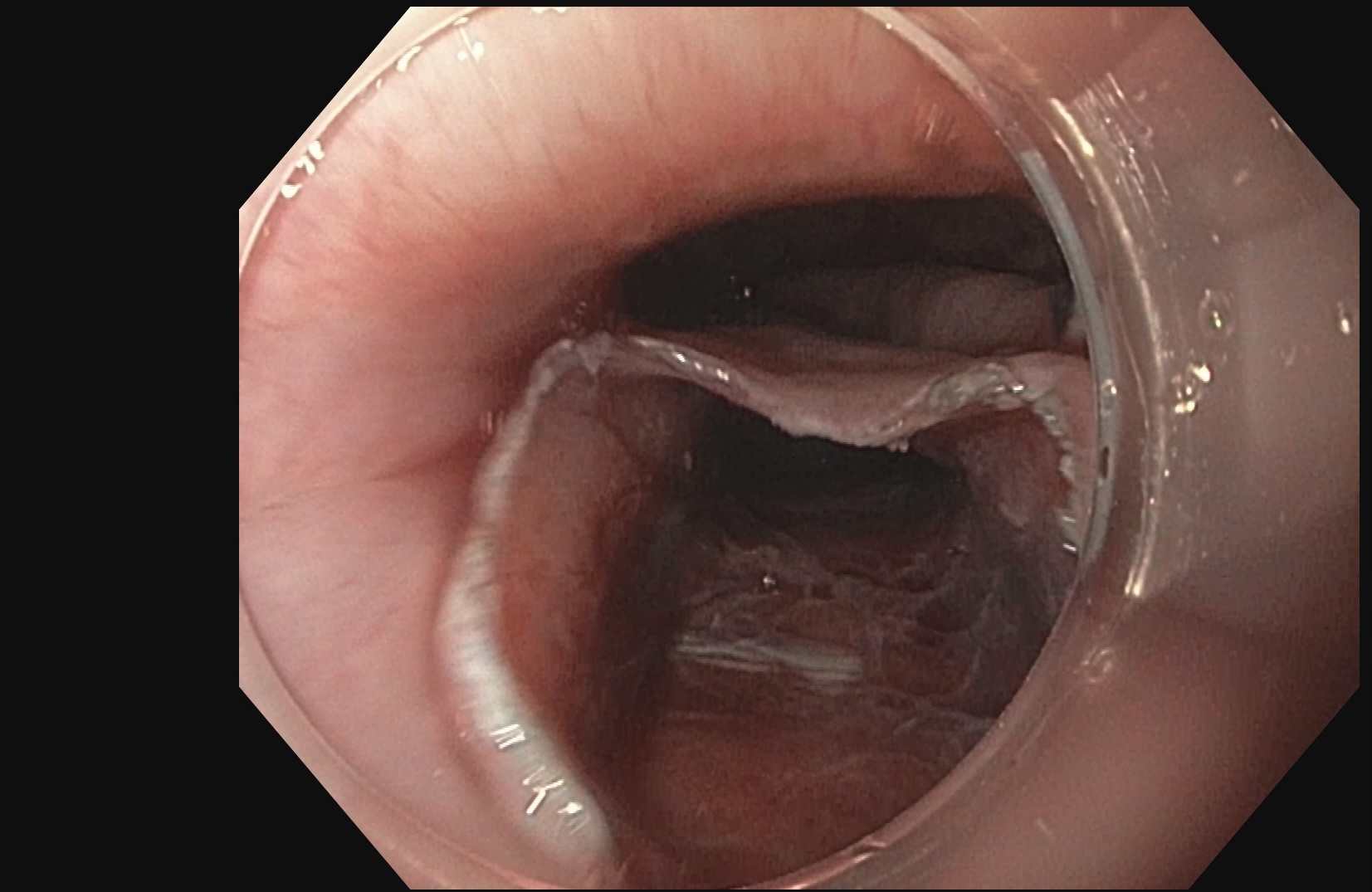
Lithotripsy is a non-invasive technique to remove gallstones that have lodged into the common bile duct and are blocking the normal flow of bile. A dye is injected into the biliary network of ducts, which is followed by an X-Ray that helps to detect the location, size, and number of stones. Ultrasound waves of a specific intensity are used to blast the stones into small granules. A stent is kept in place to remove the stone debris from the bile duct into the intestines.
A cholangiogram is a contrast study technique used to visualize the biliary network of ducts and detect the presence of any structural anomaly. The procedure involves injecting a fluorescent dye that will circulate within the biliary tree. X-Ray study is done to examine the entire biliary tree. A cholangiogram is most often indicated following surgery for the removal of the gallbladder to check for remnant stones or strictures in the biliary tract. The procedure does not require the patient to remain admitted to the hospital unless they are still recovering from the gallbladder removal surgery.
Choledoscopy is the endoscopic exploration and study of the bile duct. The purpose of the procedure is to determine the presence of the gallstones, and their subsequent removal. Choledocoscopy allows the surgeon to perform a detailed post-surgery examination of the biliary network to check if all the stones are removed. Any remnant stone debris can be removed before concluding the surgery. Due to the clear visibility that the surgeon gets of the inside of the bile duct during choledocscopy, the process has a high success rate.
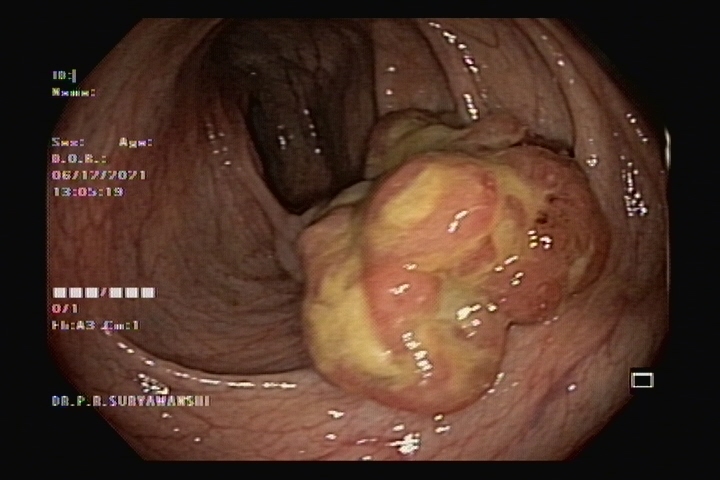
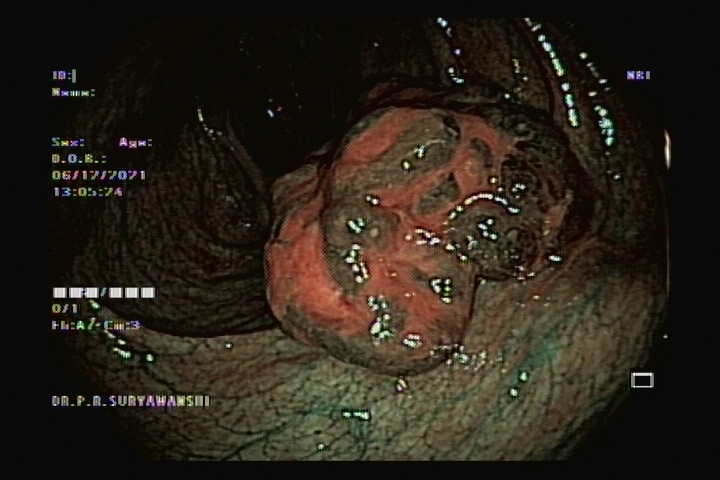
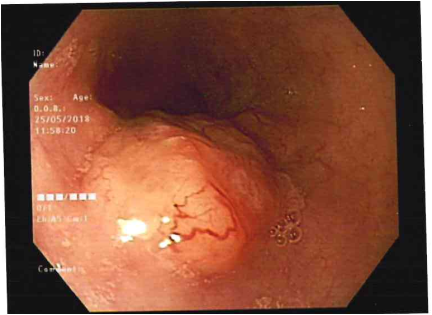
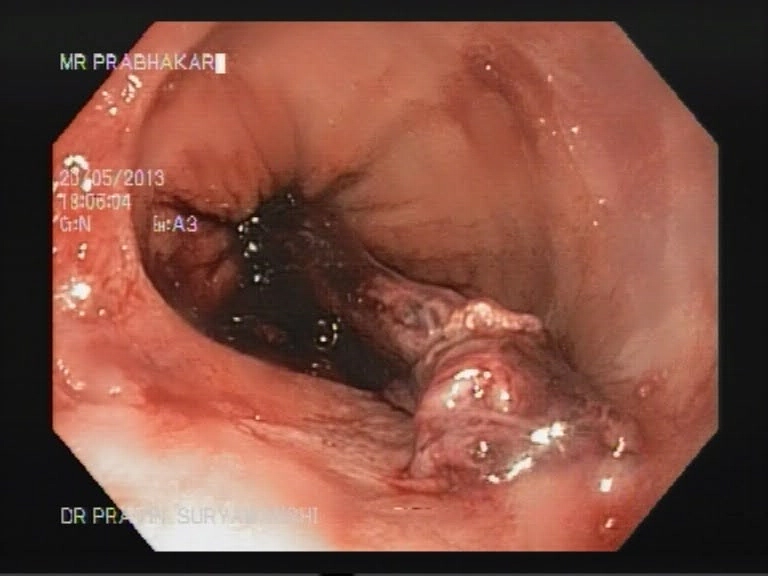
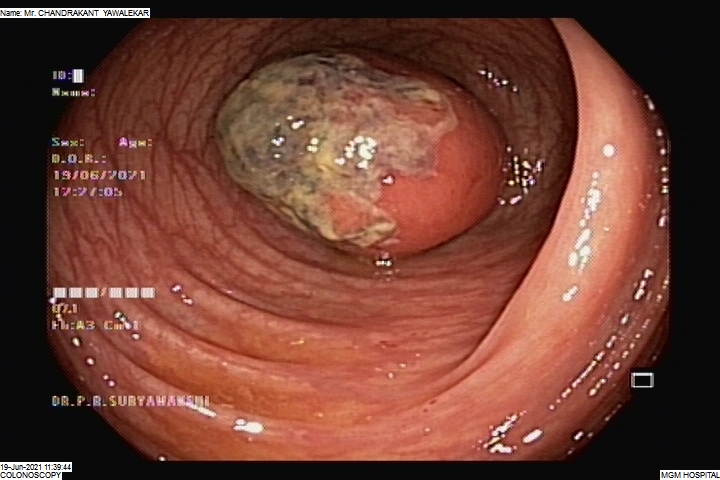
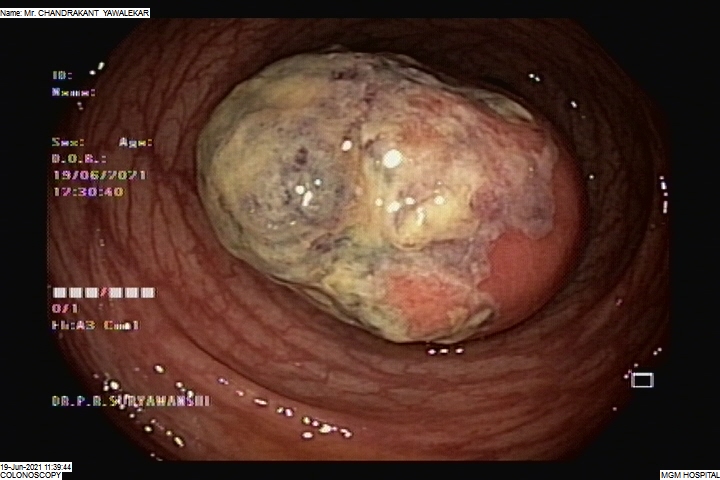
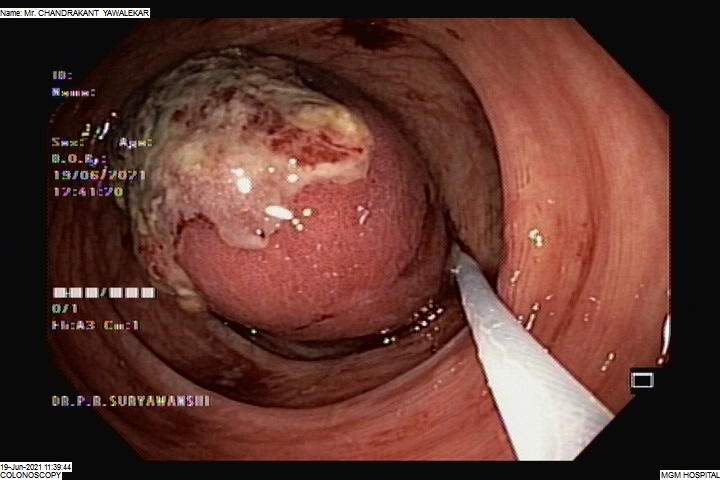
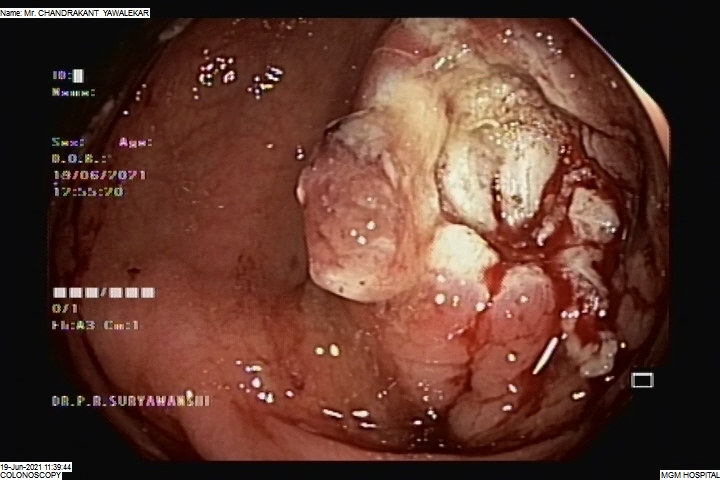
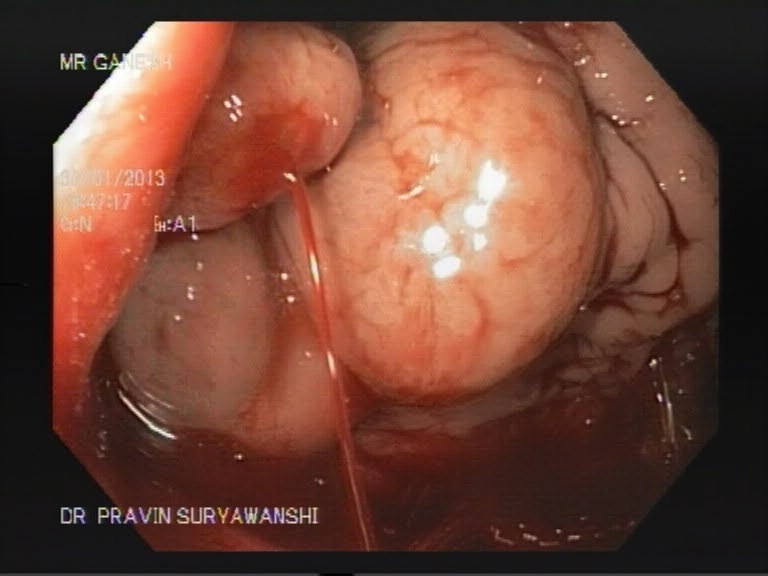
Colonic polyps are non-cancerous or cancerous tumour-like structures that grow from the colon walls and protrude inside the colonic lumen. Polypectomy is the surgical procedure performed to remove the polyps and prevent the obstruction of the colonic lumen.
During the surgery, the colonic segment where the polyps grow is isolated and adequately exposed. A colonic wall incision helps to remove the polyps, following which the wall is sutured immediately.
© 2025 All Rights Reserved